How are you doing with this recent flu wave? During the flu season, the teasing on wechat Moments came one after another: "You got vaccinated, why did you still get infected? Does the vaccine really work? We tracked some of the latest published international research findings and discovered a truth that had been misunderstood for years.
The true value of vaccines: From "preventing infection" to "saving lives"
A meta-analysis of the 2025 EUROPEAN RESPIRATORY REVIEW reveals key facts: influenza vaccines may prevent infection rates against the H3N2 strain by less than 10 percent, but still have an effect of 50 to 70 percent in reducing hospitalizations, pneumonia, and deaths. This is not a vaccine failure, but a "reinterpretation of the mechanism of action". After analyzing data from 192,000 patients, the research team found that the core value of the flu vaccine lies in reducing the severity of the disease rather than completely blocking the infection. Just as seat belts cannot prevent accidents but can determine the extent of casualties.
Why do people get vaccinated every year? The immune system's "memory trap"
A review in the Journal of Experimental Medicine has solved a 20-year mystery for the medical community. Researchers found that repeated vaccinations may cause "antigen fatigue" in the immune system. The first exposure to the virus strain leaves a deep imprint on the immune system, and more than 70 percent of the antibody response to subsequent similar vaccinations comes from "memory arousal" rather than a new immune response. Those who have been vaccinated for five consecutive years have a 30% weaker antibody response to the new variant than those who have been vaccinated for the first time. In addition, the H3N2 strain mutates very rapidly, and when the vaccine strain does not match the prevalent strain, pre-existing antibodies may interfere with the production of new protective antibodies.
This explains why vaccines often do not perform well in years when H3N2 is prevalent.
However, studies emphasize that although repeated vaccination is not perfect, it is still significantly better than not being vaccinated at all.
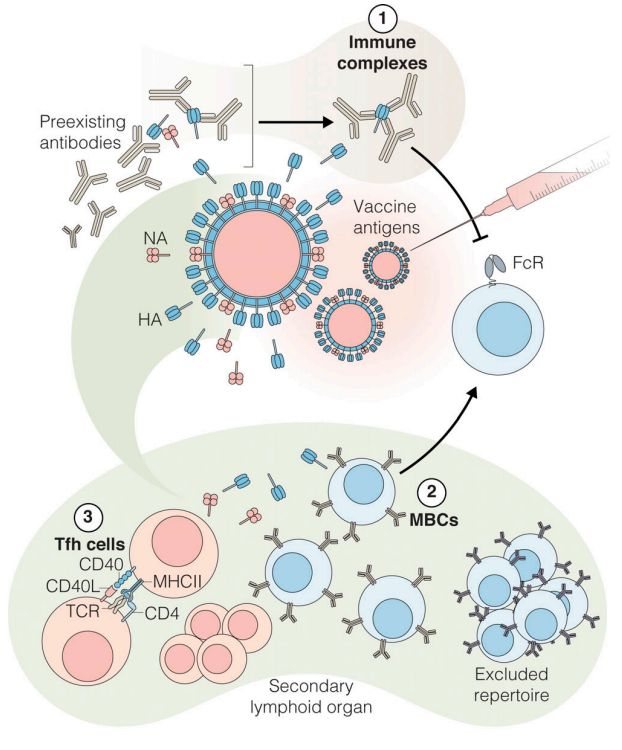
Annual influenza virus vaccine efficacy is reduced after vaccination [Matz,H.C., et.al]
Important Revelation: The time window determines life and death
During the 2009 H1N1 pandemic, Japan's flu mortality rate dropped to 0.15 per 100,000,The lowest in the world, less than half that of the United States. The success was not only due to the vaccine but also to the "48-hour golden medication strategy", according to a study by Japan's Kurashiki Central Hospital. Primary care physicians widely use rapid tests and start antiviral treatment within 48 hours of diagnosis to ensure early diagnosis and treatment for the entire population. At the same time, they have 100% access to antiviral drugs in their medical insurance coverage, and five drugs, including oseltamivir and Baloxavir, can precisely match patients' conditions in a timely manner.
Studies have shown that early administration of medication can reduce the severe illness rate by 60% and shorten the length of hospital stay by 3.2 days. This is particularly important for the elderly and patients with chronic diseases — in this population, medication administered even after 48 hours still provides significant protective value.
Special Predicament of the Elderly: Standard Vaccines May Be "Inadequate"
Due to declining physical functions and immunosenescence, the elderly mount only a 30% immune response to standard vaccines compared with young people. Enhanced vaccines show remarkable efficacy: high-dose vaccines can further reduce the risk of hospitalization by 24–59%. However, the coverage rate of enhanced vaccines remains critically inadequate — across the whole of Europe, only two countries have achieved the 75% vaccination rate recommended by the World Health Organization (WHO).
The future is here: How far are we from a universal vaccine
As we know, viral mutations are concentrated in the epitopes of surface glycoproteins — haemagglutinin (HA) and neuraminidase (NA) — particularly in the head region of HA. HA has 18 subtypes, ranging from H1 to H18, and evolves rapidly. This causes the efficacy of antibodies targeting these regions to wane as the virus evolves. Nature has reported that three revolutionary technologies have entered clinical trials.
- Immune Focusing technology- modifying the virus through a "head transplant" to replace the head of H1N1 with the H8 or H14 subtype head, thereby forcing the immune system to attack the virus’s conserved stalk. Phase I trials from the Mount Sinai School of Medicine showed that this technology can generate high levels of stalk-specific antibodies.
- Predictive vaccine design - COBRA uses AI to analyze over 100,000 virus gene sequences to predict the prevalent strains in the next five years in advance. Vaccines designed with pre-2009 data successfully protected mice from H1N1 and H3N2 strains over the next 10 years.
- T-Cell Vaccine Platform — Oregon Health & Science University utilized a cytomegalovirus (CMV) vector to deliver conserved internal viral proteins. In monkey trials, a vaccine designed based on the 1918 influenza virus surprisingly conferred protection against the modern H5N1 avian influenza virus, with a 55% protection rate.
However, scientists acknowledge that the most realistic expectation is an improved vaccine offering 3–5 years of protection, rather than a lifelong universal vaccine — the latter may never be achievable
Three tips from scientists for the current flu season
First: Correctly understand the value of the vaccine. The goal of the flu vaccine is not "zero infection", but "no severe illness". Even if infected, the symptoms are milder, recovery is faster, and it does not infect high-risk groups.
Second: Seize the 48-hour golden window. If symptoms such as high fever and muscle aches occur, it is recommended to seek medical attention and take medication within 2 days. Drugs such as oseltamivir and baloxavir can reduce the risk of severe illness by 50%.
Third: It is recommended that elderly people, pregnant women, and those with chronic diseases take the initiative to upgrade their protection.
From yearly vaccinations to longer-lasting protection with a single dose, and from preventing infection to warding off severe illness, scientific understanding of influenza vaccines is undergoing profound evolution. This winter, instead of dwelling on the question “Why do I still get a cold after vaccination?”, we should reflect: if a vaccine allows you to recover by resting at home and drinking warm water for a couple of days, rather than rushing to the emergency room in the middle of the night and throwing your whole family into chaos, then that shot is well worth taking. Ultimately, a vaccine is not meant to keep you from getting sick at all — it is meant to keep you from fearing illness when it does strike.
[1] Presa J, et al. Influenza vaccine outcomes: a meta-analysis revealing morbidity benefits amid low infection prevention. Eur Respir Rev. 2025; 34 (175) : 240144. Doi: 10.1183/16000617.0144-2024
[2] Matz HC, et.al. Vaccination against influenza viruses annually: Renewing or narrowing the protective shield? . J Exp Med. 2025; 222(7):e20241283. doi:10.1084/jem.20241283
[3] Bonomini A, et.al. Antiviral strategies against influenza virus: an update on approved and innovative therapeutic approaches. Cell Mol Life Sci. 2025; 82(1):75. doi:10.1007/s00018-025-05611-1
[4] Ishida T. Antiviral treatment for influenza in Japan. J Infect Chemother. 2025; 31 (8) : 102760. Doi: 10.1016 / j.j iac. 2025.102760
[5] Gavazzi G, et al. Enhanced influenza vaccination for older adults in Europe: a review of the current situation and expert recommendations for the future. Expert Rev Vaccines. 2025; 24 (1) : 350-364. The doi: 10.1080/14760584.2025.2499728
[6] Neil Savage, A universal flu vaccine has proved challenging — could it finally be possible? https://www.nature.com/articles/d41586-025-03608-1
